Electro-Capacitive Cancer Therapy (ECCT) is an innovative and non-invasive cancer treatment that leverages the effects of electric fields (EF) on cellular activity. ECCT specifically targets the electrical characteristics of cancer cells, which differ from those of healthy cells. Cancer cells exhibit abnormal electrical behaviour, especially during mitosis (cell division), where their electrical properties can be exploited to disrupt cell proliferation. ECCT delivers carefully controlled electric fields at intermediate frequencies to selectively interfere with cancer cell division while sparing normal cells, making it a promising approach in cancer treatment. Unlike conventional methods like chemotherapy and radiation, which often affect both cancerous and healthy tissues, ECCT offers a more targeted therapy with potentially fewer side effects.
The importance of optimizing ECCT for effective treatment lies in its ability to maximize the impact on cancer cells while minimizing unintended effects on surrounding healthy tissue. The efficacy of ECCT depends on how accurately the electric fields are applied to the tumor site. Variables such as tumor size, location, and the properties of the surrounding tissue can significantly influence treatment outcomes. Without precise control and optimization, electric fields may not reach the necessary intensity to disrupt cancer cells or may affect healthy tissues, reducing the overall effectiveness of the treatment. Therefore, optimizing ECCT involves refining treatment parameters to ensure that electric field intensity is distributed in a way that maximally impacts cancer cells while sparing normal tissue [1].
This blog will focus on understanding how electric field (EF) distribution affects treatment outcomes in ECCT. By examining how EF interacts with different types of tissue and the role of dielectric properties (how materials respond to electric fields), researchers can improve the design and application of ECCT. In particular, this article will explore the use of Wire Mesh Tomography (WMT) to measure EF distribution in various media, offering insights into how this technique can help refine and optimize ECCT for more effective cancer treatment. Understanding EF distribution is crucial because it not only enhances treatment accuracy but also ensures that cancer cells receive the maximum therapeutic benefit, leading to improved patient outcomes.
Electro-Capacitive Cancer Therapy (ECCT) is based on the principle that cancer cells exhibit distinct electrical properties compared to normal, healthy cells. ECCT harnesses this difference by using externally applied electric fields (EF) to inhibit cancer cell growth and proliferation. In essence, ECCT generates electric fields that interfere with the abnormal electrical activity of cancer cells, especially during critical stages like mitosis, when cells are actively dividing [2]. The electric fields used in ECCT are typically tuned to intermediate frequencies, which have been shown to disrupt key cellular processes in cancer cells without significantly affecting the surrounding normal cells.
The mechanism by which ECCT inhibits cancer cell growth involves the interaction between electric fields and the biophysical characteristics of the cells. Cancer cells, due to their uncontrolled growth and division, have altered membrane potentials, ion channel activity, and overall electrical conductivity compared to normal cells. These differences in electrical properties make cancer cells more susceptible to disruption by externally applied electric fields.
In ECCT, the electric fields target the cancer cells’ abnormal activity by interfering with their mitotic spindle formation during cell division. Mitosis is a highly regulated process, and any disruption to the spindle apparatus can lead to failed division or even cell death. By applying electric fields at specific intensities and frequencies, ECCT selectively affects cancer cells’ ability to divide, effectively halting tumor growth. Importantly, healthy cells, which maintain more stable electrical properties and undergo less frequent division, are far less impacted by these fields, making ECCT a selective and targeted therapy [3].
One of the key advantages of ECCT is this ability to exploit cancer cells’ vulnerabilities without causing significant damage to normal tissues. Unlike chemotherapy or radiation, which damage both healthy and cancerous tissues, ECCT focuses primarily on cells that display abnormal electrical behavior. This selectivity not only enhances the treatment’s effectiveness but also reduces side effects, offering a less invasive alternative to conventional cancer treatments. Moreover, ECCT has been studied for its potential to work synergistically with other treatments, potentially improving patient outcomes across a variety of cancer types.
The Importance of Electric Field Distribution in ECCT
In Electro-Capacitive Cancer Therapy (ECCT), the distribution and intensity of electric fields (EF) play a crucial role in determining the therapy’s effectiveness. The success of ECCT in inhibiting cancer cell growth relies on the precise application of electric fields, which disrupt critical cellular processes such as mitosis. Mitosis, the process through which cancer cells divide, is highly sensitive to external electric forces. By carefully controlling the intensity and distribution of electric fields, ECCT can interfere with mitotic spindle formation, leading to failed cell division and, ultimately, cancer cell death [4]. EF intensity is critical because different tissues and cells respond variably to electric fields. Cancer cells, due to their irregular growth, have altered electrical properties, including differences in membrane potential and conductivity, which make them more susceptible to electric field interference. During mitosis, when cancer cells are actively dividing, they are particularly vulnerable to changes in their electrical environment. A carefully calibrated electric field can destabilize the mitotic spindle apparatus, causing the division process to stall or fail. Without proper cell division, cancer cells either die or become nonviable, slowing tumor growth and spread. To achieve optimal results, electric field intensity must be carefully managed to ensure that it reaches the cancerous tissue with enough strength to disrupt mitosis. At the same time, the surrounding healthy tissue, which has different electrical properties, should remain largely unaffected. The key is finding the right balance: fields that are strong enough to halt cancer cell proliferation while being weak enough to avoid harming normal cells. Previous studies have shown that the selective nature of EF intensity in ECCT allows for this precision. For example, research has demonstrated that electric fields at intermediate frequencies preferentially affect cancer cells due to their abnormal electrical activities. These fields can target cancer cells by exploiting the differences in dielectric properties between cancerous and healthy tissues. As cancer cells have higher conductivity and different dielectric constants, they respond more intensely to electric fields than normal cells. This preferential targeting is one of the most significant advantages of ECCT because it reduces collateral damage to healthy tissues, unlike traditional treatments such as radiation or chemotherapy, which tend to damage both cancerous and healthy cells [5]. In addition, studies have also highlighted how variations in the surrounding tissue medium, such as differences in conductivity and permittivity, can affect the distribution and efficacy of electric fields. By understanding how electric fields behave in different tissue environments, researchers have been able to fine-tune ECCT protocols to maximize therapeutic benefits. For example, simulations and experiments using tumor phantoms (models of tumor tissue) have shown that electric field distribution can be optimized by accounting for the properties of both the tumor and its surrounding tissue. This allows for more precise targeting of cancer cells and improved treatment outcomes.Simulation and Measurement of EF Distribution
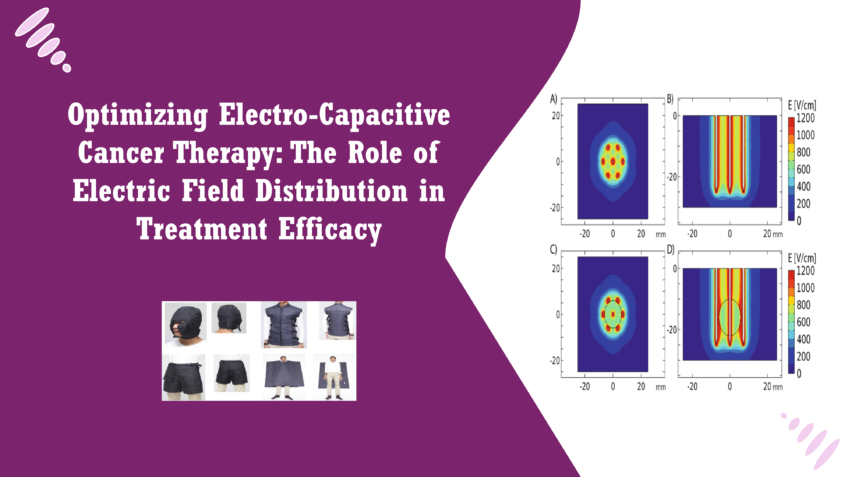
Scientists used WMT to measure the distribution of electric fields in a simulated cancer treatment scenario. The researchers employed tumor phantoms, which are artificial models of tumor tissue, to investigate how EF is distributed in different environments. These phantoms were surrounded by two different media—air and silicone—to simulate the effects of various tissue environments on electric field propagation. Air and silicone were chosen for their distinct dielectric properties, which represent the variability of tissues in the human body. The goal was to determine how this different surrounding media affect EF distribution and, by extension, the effectiveness of ECCT in targeting cancer cells [6]. The WMT measurements provided real-time data on the electric field intensity within the tumor phantoms and the surrounding media. By observing how EF intensity varied across different regions, the researchers were able to better understand how electric fields behave in different dielectric environments. For example, EF intensity tends to drop off at the boundary between the tumor and surrounding media, meaning that the properties of the surrounding tissue can significantly impact treatment efficacy. To validate the accuracy of these WMT measurements, the researchers conducted computational simulations that modeled the same experimental setup. These simulations aimed to replicate the EF distribution observed in the WMT experiments, using computational algorithms to predict how electric fields would propagate in the same tumor and media configurations. The computational models were compared with the actual measurements obtained from the WMT experiments. The results from research showed that the WMT measurements and computational simulations were in close agreement, confirming that the wire mesh tomography method is reliable for capturing EF distribution. Both the measured and simulated data demonstrated similar trends in EF intensity, particularly at the boundary regions where the tumor phantom met the surrounding media. This validation is critical, as it confirms that WMT can be used as an accurate tool for assessing and optimizing EF distribution in ECCT treatments [7]. In the research experiment, the surrounding media—air and silicone—significantly affected the distribution of electric fields (EF) around the tumor phantoms. These media represent different types of tissue environments in the body, each with distinct dielectric properties that influence how electric fields propagate. When the tumor phantom was surrounded by air, which has a low dielectric constant, the EF intensity around the tumor was higher and more concentrated. This is because air, as a poor conductor of electric fields, allows the field to remain strong around the tumor without much dissipation. As a result, the electric field gradient—how quickly the field strength changes across space—was steep, with a sharp drop in EF intensity near the boundary of the tumor. Conversely, when the tumor phantom was surrounded by silicone, which has a higher dielectric constant and conductivity, the EF intensity was more dispersed. Silicone, acting like a conductive tissue medium, absorbed some of the electric field, causing a more gradual decline in field strength at the boundary between the tumor and the surrounding medium. This led to a less pronounced EF gradient. The results from both environments highlighted that the surrounding tissue’s dielectric properties play a critical role in how effectively the EF can target the tumor [8]. Understanding how EF distribution is affected by different tissue environments is crucial for optimizing Electro-Capacitive Cancer Therapy (ECCT). Since electric fields interact with tissues based on their dielectric properties, the effectiveness of ECCT can vary depending on the type of tissue surrounding the tumor. For example, tumors surrounded by more conductive tissues may require different EF intensities or treatment frequencies to achieve the same level of therapeutic efficacy as tumors in less conductive environments. The research demonstrates that by carefully measuring EF distribution using tools like Wire Mesh Tomography (WMT) and validating these measurements through computational simulations, clinicians can fine-tune ECCT treatments to account for the specific tissue environment of each patient. This level of customization could enhance the targeting of cancer cells, ensuring that the electric fields are strong enough to disrupt cell division without affecting healthy tissues nearby. By taking into account the dielectric properties of the surrounding tissue, ECCT treatment plans can be adapted to ensure that electric fields are applied effectively. For example, tumors located in denser or more conductive tissues may require adjustments in field strength or frequency to maintain the therapeutic effects seen in more favorable tissue environments. This type of optimization not only improves treatment accuracy but also enhances the overall efficacy of ECCT [9].Conclusion
The optimization of electric field distribution is a key factor in enhancing the efficacy of Electro-Capacitive Cancer Therapy (ECCT). By measuring and understanding how electric fields behave in different tissue environments, clinicians can improve the precision of ECCT treatment, ensuring that electric fields are applied with maximum therapeutic benefit. The differences in dielectric properties between the tumor and surrounding tissue significantly impact how electric fields are distributed and how effectively they can target cancer cells during mitosis. The blog highlighted the importance of tools like Wire Mesh Tomography (WMT) and computational simulations in improving ECCT treatment planning. These methods provide valuable insights into how electric fields interact with varying tissue types, allowing for adjustments that can make ECCT more effective for a broader range of cancer patients. As ECCT continues to develop as a promising cancer therapy, further research and technological advancements are needed to refine these techniques. Improved measurement tools, more advanced simulations, and a deeper understanding of tissue-specific electric field interactions will help make ECCT a more versatile and widely applicable treatment for diverse cancer types, ultimately improving patient outcomes and advancing the field of non-invasive cancer therapies.References
- A. Mujib, F. Alamsyah and W. P. Taruno, “Cell Death and Induced Expression in Oral Cancer HeLa and Bone Marrow Mesenchyme Cells under the Exposure to Noncontact Electric Fields”, Integr. Med. Int, vol. 4, no. 3, pp. 161-170, Dec. 2017.
- P. Taruno, Kapasitif Elektro Terapi (Alat Terapi Penyakit Kanker), vol. 2013, pp. 03941, 2017.
- D. Kirson et al., “Disruption of cancer cell replication by alternating electric fields”, Cancer Res, vol. 64, no. 9, pp. 3288-95, May 2004.
- Alamsyah, I. N. Ajrina, F. N. A. Dewi, D. Iskandriati, S. A. Prabandari and W. P. Taruno, “Antiproliferative Effect of Electric Fields on Breast Tumor Cells In Vitro and In Vivo”, Indones. J. Cancer Chemoprevention, vol. 6, no. 3, pp. 71, Jan. 2017.
- Giladi et al., “Alternating Electric Fields (Tumor-Treating Fields Therapy) Can Improve Chemotherapy Treatment Efficacy in Non-Small Cell Lung Cancer Both In Vitro and In Vivo”, Semin. Oncol, vol. 41, pp. S35-S41, Oct. 2014.
- Prasser, D. Scholz and C. Zippe, “Bubble size measurement using wire-mesh sensors”, Flow Meas. Instrum. elsevier, vol. 12, pp. 299-312, 2001.
- J. Azzopardi et al., “Comparison between Electrical Capacitance Tomography and Wire Mesh Sensor Output for Air/Silicone Oil Flow in a Vertical Pipe”, Ind. Eng. Chem. Res, vol. 49, no. 18, pp. 8805-8811, 2010.
- Chen, Y. Ji and N. Jin, Study on Image Reconstruction Algorithms for Wire Mesh Tomography System, Berlin, Heidelberg:Springer, pp. 133-138, 2012.
- Handriyanto, Electro-Capacitive Cancer Treatment (ECCT) Effectiveness for Brain Cancer, 2013.